Up to 50% of U.S. women experience some degree of urinary incontinence, or the involuntary leakage of urine, with the prevalence increasing as women age. Due to embarrassment, lack of education and concern about treatment options, many women fail to seek help, or delay treatment for several years, negatively impacting their quality of life in the meantime. In many cases, lifestyle changes and simple medical care can bring about improvements in this condition for women.

Sneeze

Exercise

Laugh

Cough

Walk
Bladder Leakage & Incontinence Support
Incontinence is more common in women, with causes that are often related to pregnancy, childbirth, menopause and other changes that impact the pelvic floor. Understanding the type of incontinence you are experiencing helps your health care provider determine the most appropriate treatment options for you. They include:
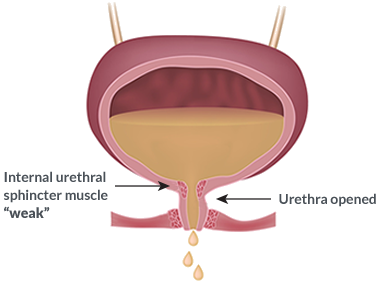
- Stress incontinence: Occurs when pressure on the bladder from actions such as coughing, sneezing, laughing, exercising, or lifting heavy objects causes it to leak urine.
- Urge incontinence: This is defined as a sudden, intense urge to urinate, followed by involuntary urine leakage. A condition called overactive bladder (OAB) can be the cause of this type of incontinence.
- Overflow incontinence: This type of incontinence involves frequent or constant dribbling of urine due to the bladder not fully emptying.
- Functional incontinence: Occurs when you are prevented from getting to the bathroom in time by physical or mental limitations. For example, severe arthritis might make it difficult to unbutton your pants quickly enough.
- Mixed incontinence: This is a combination of different types of urinary incontinence, most commonly, stress and urge incontinence, together.
Advantia Health and its women’s health providers offer a range of personalized treatment options that range from lifestyle changes to surgery, depending on the type of incontinence you’re experiencing, and the reasons for it.
Diagnosis and Treatment for Incontinence
A first visit to your healthcare provider about bladder control issues will likely begin with a discussion about your medical history, diet and lifestyle, medications you take, and your experiences with incontinence. That information will enable your provider to identify the type of incontinence you may have, and the tests most appropriate to diagnose it.
Your provider may ask you to keep a journal about the frequency with which you urinate, activities that cause leakage, and similar details at home to help supplement in-office tests or exams.
Diagnostic test options include:
- Pelvic exam to identify possible physical causes
- Urinalysis to check for urinary tract infection
- Bladder ultrasound to determine how well your bladder empties itself
- Stress test to identify bladder leaks that occur during coughing or similar actions
- A pad test, to see how much urine your bladder is leaking
- Urodynamic testing, which is a series of tests that check how much fluid your bladder can hold and how well your muscles hold your urethra shut
- Cystoscopy, where a camera is inserted into your urethra to closely examine your urinary tract
Depending upon your diagnosis, treatment options for incontinence include (1) medications, including hormone replacement therapies and those specially designed to strengthen or relax the muscles that control bladder function, (2) lifestyle changes, including diet and exercise, and (3) surgical procedures.
Tailored Pelvic Floor Therapy
Pelvic Floor Muscle Training (PFMT) is a non-surgical, painless method of retraining the pelvic floor muscles that help control bladder, bowel, and sexual function. Like other muscles in your body, your pelvic floor muscles will become stronger with a repetitive exercise program. Strengthening those muscles will help you to actively support your bladder and bowel, reducing the likelihood of leaking.
A specialist trained in PFMT will teach you how to isolate your pelvic floor muscles, and instruct you on how to perform the pelvic muscle exercises. The provider will determine the treatment best suited for you and prescribe a course of therapy for your specific condition.
Managing Bladder Leakage
There are a number of lifestyle changes you can implement at home to help you manage urinary incontinence and prevent leakage. You should check with your provider to ensure your changes align with your diagnosis and that you are performing activities properly.
These changes can include:
- Emptying your bladder before physical activity or on a regular schedule (timed voiding).
- Bladder training to extend the amount of time that passes between each trip to the bathroom.
- Regularly exercising your pelvic floor muscles through Kegel exercises. It is crucial that these are done correctly to strengthen the right muscles,so you may wish to see a trained therapist.
- Avoiding caffeine, tobacco, alcohol, carbonated beverages and other foods that can irritate your bladder, and increasing fiber consumption to prevent constipation.
- Maintaining a healthy body weight, as excess body weight can cause incontinence.
- Not lifting heavy objects.
- Wearing products designed to discreetly capture leaked urine.
Once you have exhausted less-invasive treatment options, your healthcare provider may recommend a surgical intervention for treating urinary incontinence. These options can include:
- Bulking agents, like Bulkamid, which is specifically designed to assist with stress incontinence through an injection that increases the size of the urethra.
- Botox injections in your bladder to help relax the muscles and reduce urge incontinence.
- Neuromodulation devices, which are pacemakers that can be implanted to help stimulate the nerves of the bladder and improve bladder control.
- Sling procedures, which use synthetic material or your body’s own tissue to support the urethra.
Other Related Incontinence Issues
Bladder leakage may result in various challenges that affect both physical and emotional well-being, such as skin irritation, infections of the urinary system, and mental health concerns. It can also interfere with daily routines, social engagement, and general life satisfaction.
In many instances, there are non-invasive or minimally invasive treatment options that can help you increase your comfort and quality of life. Talk to your healthcare provider to learn how to minimize the impact of urine leakage.
Advantia Health Expertise
Many Advantia Health providers offer innovative, effective solutions for bladder leakage and incontinence. Call your nearest office or explore trusted affiliate providers listed on this page.